Medication-related osteonecrosis of the jaw using periodontitis-induced rat before tooth extraction | BMC Oral Health | Full Text
In this study, 24 skeletally mature, 12-week-old, female Sprague-Dawley rats (Orientbio Co., Ltd.; Seongnam-si, Gyenggi-do, Korea) were used. The mean weight of the animals was 281 g at 12 weeks of age and 421 g immediately before sacrifice. The animals were housed under standard laboratory conditions (temperature, 20 °C ± 5 °C; humidity, 50% ± 10%; lighting cycle, 12 h light/12 h dark), with 2–3 rats per cage and marked individually. All animals had ad libitum access to standard laboratory pellet diet and water. This investigation was carried out in accordance with the revised animals Act 1986 in the UK used for scientific procedure, and confirm the study complied with the ARRIVE guidelines. Animal selection, management, surgical protocol, and preparation followed a routine protocol approved by the Institutional Animal Care and Use Committee of Yonsei University Health System (IACUC No. 2016 − 0171).
Experimental design
These 24 animals were randomly divided into two groups administered with saline (CONT group, N = 13) and zoledronic acid (ZA) (ZA group, N = 11), respectively (Fig. 1). Based on the results of the pilot study, the sample size was calculated, and G-power 3.1 was used. This was set at an effect size of 0.5, significance of 0.05, and power of 90%. Considering the dropout rate of 20%, 13 animals per group were finally calculated. At 12 weeks of age, bilateral ovariectomy (OVX) was performed in all animals under general anesthesia by intraperitoneal combination injection of tiletamine and zolazepam (50 mg/mL, 0.6 mL/kg; Zoletil®, Virbac Lab. Carros, France) and xylazine (23.32 mg/mL, 0.4 mL/kg; Rompun®, Bayer, Leverkusen, Germany). The OVX procedure is as follows: After shaving the spine, such as the lower abdomen, disinfect it. Afterwards, a 15 mm incision is made in the skin and a 5 mm incision is made in the peritoneum where the left/right ovary is located. The OVX is performed by exposing the ovary, and the remaining organs are placed back into the peritoneum. The peritoneum is not sutured, only the dorsal skin is sutured.
Experimental design protocol and clinical photographs of tooth ligation for inducing periodontitis
Postoperatively, meloxicam (1 mg/kg, once a day for 5 days; Metacam®, Boehringer Ingelheim, Rhein, Germany) and enfloxacin (10 mg/kg/day, once a day for 5 days; Baytril®, Bayer, Germany) were administered subcutaneously (SC).
Eight weeks later, 4 − 0 black silk ligation was performed on the cervical portion of the right mandibular first molar (M1) and second molar (M2) under general anesthesia in all rats (Fig. 1). Four weeks later, ZA (Zometa ready®, Novartis, Basel, Switzerland; 40 µg/kg, once a week for 4 weeks) was administered in the ZA group and saline (same volume as ZA) in the CONT group intravenously (IV) [29, 30].
Eight weeks later, silk remove with tooth extraction was performed under general anesthesia in all animals. Clinical observations such as gingival tenderness and tooth mobility around the ligated teeth were made before tooth extraction and silk removal. Local anesthesia was induced using 2% lidocaine (1: 80,000 epinephrine). The ligated right mandibular M1 and M2 were extracted using a sharp dental explorer after ensuring sufficient mobility. Bleeding was controlled by gauze pressure, and suturing was not required. After tooth extraction, meloxicam and enfloxacin were administered SC to prevent postoperative infection and achieve pain control.
All animals were sacrificed 8 weeks after tooth extraction by perfusion under general anesthesia. After removing the skin, the organs were extracted and fixed in 10% formalin.
Micro-computed tomography (micro-CT)
Ten specimens (CONT group, N = 5; ZA group, N = 5) were subjected to micro-CT (Skyscan1173, Skyscan, Konitch, Belgium) at 100 kV, 100 µA, and 13.86 μm pixel size in the tibia and 18.12 μm pixel size in the jaw. CTAn (Skyscan, Aartselaar, Belgium) was used to reconstruct and analyze the images.
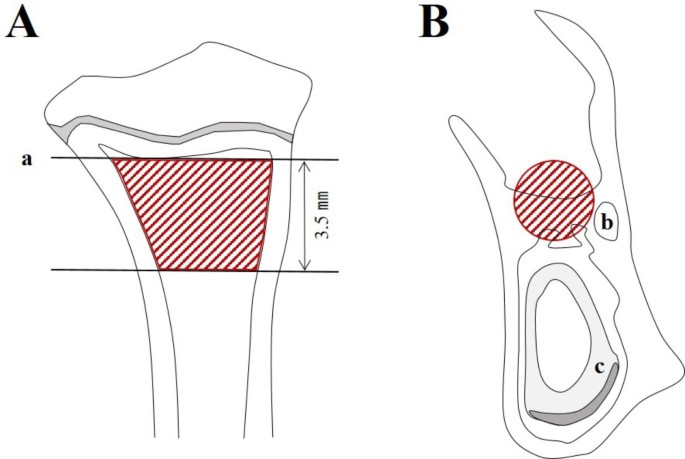
For the trabecular bone morphometry of the tibia, the region of interest (ROI) in the tibia was the growth plate and 3.5 mm of the upper trabecular bone (Fig. 2A and a) [31]. For the trabecular bone morphometry of the extraction site, the ROI was the interradicular bone of Ø0.6 mm-sized cylindrical shape in the coronal view (Fig. 2B, b and c). The posterior border was the mesial root surface of the third molar, and the anterior border was considered 4 mm from the posterior border.
ROI in micro-CT analysis. A Proximal tibia, B EXT site. a Growth plate, b Mandibular canal, c Incisor root (ROI, red area)
Abbreviations: ROI = region of interest, Micro-CT = micro-computed tomography, EXT = extraction
All specimens were decalcified using 10% ethylenediaminetetraacetic acid, embedded in paraffin, and 4-µm serial coronal sections were obtained. Hematoxylin and eosin staining was performed according to the manufacturer’s recommendations. Images were scanned using a light microscope (Case Viewer, 3DHISTECH Ltd., Budapest, Hungary). Histologically, MRONJ was diagnosed when one or more of the following signs were observed: exposed bone, necrotic bone, inflammatory infiltration, or sequestrum [33].
Statistical analysis
Statistical analyses were performed using Statistical Product and Service Solutions (IBM SPSS 23.0, IBM Corp., Armonk, NY, USA). Mann-Whitney U-test and chi-squared test were used to compare parameters between the CONT and ZA groups; p-values < 0.05 were considered statistically significant.

… [Trackback]
[…] Read More to that Topic: pache.co/2023/08/29/medication-related-osteonecrosis-of-the-jaw-using-periodontitis-induced-rat-before-tooth-extraction-bmc-oral-health-full-text/ […]
… [Trackback]
[…] There you can find 60524 more Information to that Topic: pache.co/2023/08/29/medication-related-osteonecrosis-of-the-jaw-using-periodontitis-induced-rat-before-tooth-extraction-bmc-oral-health-full-text/ […]
… [Trackback]
[…] Find More to that Topic: pache.co/2023/08/29/medication-related-osteonecrosis-of-the-jaw-using-periodontitis-induced-rat-before-tooth-extraction-bmc-oral-health-full-text/ […]